 27
27Aug
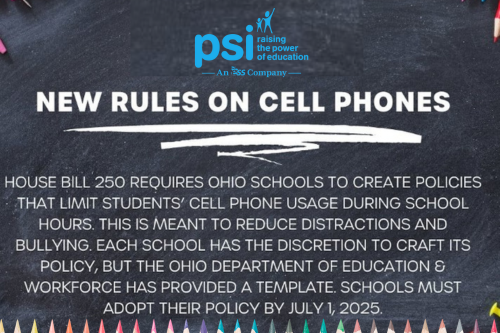
Cell Phones in Schools
The debate over whether or not students should be allowed to use their cell phones throughout the school day is intense. School administrators, psychologists, and teachers argue that phones are a distraction, and their constant use is contributing to this generations academic and mental health decline. But with the rising incidence of deadly school shootings […]
 05
05Feb
CMS Announces $50 Million in Grants to Deliver Critical School-Based Health Services to Children
Grants will help up to 20 states implement or expand school-based health services for children enrolled in Medicaid and CHIP On January 24, 2024 the U.S. Department of Health and Human Services (HHS), through the Centers for Medicare & Medicaid Services (CMS), announced $50 million in grants for states to connect millions more children to […]
 05
05Feb
How virtual nursing can help solve many workforce shortage woes
One of the nurse executives who helped create the world’s first virtual hospital offers a deep dive into the benefits of a hybrid approach to nursing that employs telehealth. Hospitals across the nation are facing workforce challenges, and a nurse staffing shortage poses one of the biggest threats to care delivery. More than 100,000 nurses exited the U.S. […]
 05
05Feb
There’s a strong push for more school psychologists
A combination of pre-existing shortages and a rise in school stressors has led to a major effort to train and hire more mental health professionals for school settings. With a growing mental health crisis among young people—a trend both exacerbated and illuminated by COVID—the need for school psychologists is multiplying. School psychologists in the United […]
 05
05Feb
CDC Mental Health and Well-Being Action Guide for Schools
The CDC has recently developed a new action guide for mental health and well-being for schools. Please see a brief description below and follow the links for more important information. CDC recently released a school mental health action guide to support schools in their efforts to promote students’ mental health. This action guide is a direct […]
 05
05Dec
Exciting News at PSI
We are delighted to announce that PSI has become a part of Education Solutions Services (ESS), a leading and highly respected firm in the education industry. This strategic partnership marks a significant milestone in our company’s journey and opens up new opportunities for improvements to our recruiting process, continued innovation, and enhanced collaboration. Steve Rosenberg […]
 29
29Nov
Scholarship Winner – Rose Rife
We are delighted to announce that Rose Rife has been selected as the winner of the annual 2023 School Psychology $1,000 Scholarship Award by PSI. Rose is completing her internship and is in her 3rd year in the School Psychology program at Cleveland State University. She has demonstrated an unwavering commitment to enhancing the lives […]
 28
28Nov
PSI is excited to announce that Steve Rosenberg, Ph.D., will be recognized at the 2023 Smart 50 Awards
PSI is excited to announce that Steve Rosenberg, Ph.D., will be recognized at the 2023 Smart 50 Awards, hosted by @Smart Business Network and presented by @Corporate College. The Smart 50 Awards recognized the top executives of the 50 smartest companies in Northeast Ohio for their ability to effectively build and lead successful organizations! PSI […]
 28
28Nov
Ohio ranks near top of states for school voucher spending
Ohio’s increase in school voucher spending this year for the EdChoice Expansion Program sets up the state to rank near the top nationally when it comes to taxpayer use of voucher dollars to attend private schools. This is not only because of the increase in voucher money for each child but also because of an […]
 28
28Nov
The Top 10 Elementary, Middle Schools in Ohio
The U.S. News & World Report released a ranking of Ohio’s top elementary and middle schools Thursday, assessing nearly 80,000 schools across the country. Each year, U.S. News & World Report has traditionally released a ranking list of high schools and universities in the country, and this year, they are also ranking elementary and middle […]
Recent Comments