 01
01Nov
A Heartwarming Tale of Heroism
We wanted to share with you a remarkable incident that unfolded at one of our
partner schools recently. One of our dedicated nurses, Rachel Ocampo, played a
pivotal role in saving the life of one of the students.
 01
01Nov
PSI at 100+ Latinos CLE Must Know Meet and Greet
Milagros Zavalia and Amanda Mooney represented PSI at AmMore Consulting’s 100+ Latinos CLE Must Know Meet and Greet at the Cleveland Zoo on Friday night.
 18
18Aug
The impact of Ohio’s new education laws
Back to school: How Ohio’s new education laws will impact parents, teachers and students
 07
07Aug
Spotlight on #TeamPSI
Some great stories about some great PSI employees!
 22
22Apr
The Skin You’re In
Typically making its unwelcome arrival during puberty, acne ranges from small whiteheads to painful cystic lesions. Over-the-counter medications usually contain astringents, agents that help to dry out oily skin. Active ingredients include witch hazel, rubbing alcohol, or even salicylic acid. Astringents work by removing oil and unclogging the skin’s pores. More recently, medications with […]
 17
17Feb
Screentime & the Developing Brain
Earlier this month, a study published by Harvard University’s Center for the Developing Child concluded that letting infants watch tablet, phone, and TV screens might have negative effects on their academic achievement and emotional well-being down the road. This long-term study evaluated nearly 500 children using an EEG at 1, 1-1/2, and 9 years of […]
 16
16Feb
Vaping Guidance: What Parents Need to Know
From 2011 to 2019, the CDC reported a 900% increase in vaping for teens in high school. Vaping refers to the inhalation of aerosolized particles of a drug (marijuana or nicotine), mixed with flavoring. Most vaping devices contain a battery for power, a heating element, a place to insert the drug-containing liquid that will be […]
 04
04Feb
What’s new in COVID boosters?
The FDA has approved an emergency use authorization for a new bivalent booster shot to aid in the fight against COVID-19. Here’s what you need to know about these new vaccines. Q: What is a bivalent vaccine? A: Bivalent refers to the two separate virus strains whose mRNA instructions are included in the new booster […]
 01
01Feb
In Case of Emergency with Dr. Carly Wilbur
Would you know how to respond in an emergency situation? Some of us learned CPR in high school or for a babysitting class, but how many adults keep up with these skills? No one ever plans to be in an emergency situation, but quick thinking in a crisis can potentially mean the difference between life […]
 26
26Jan
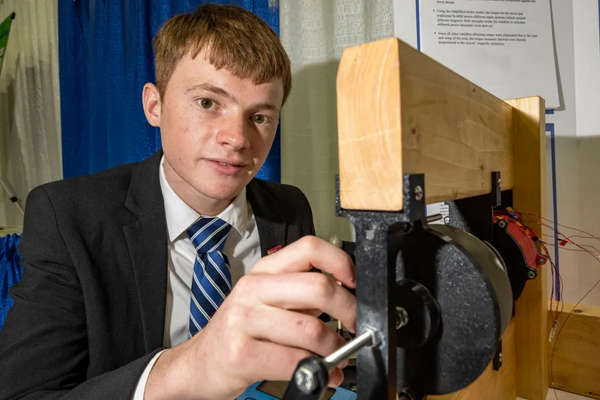
Teen Invents World’s First Sustainable EV Motor
Robert Sansone’s research could pave the way for the sustainable manufacturing of electric vehicles that do not require rare-earth magnets – and he’s only 17 years old! Robert Sansone is a natural born engineer. From animatronic hands to high-speed running boots and a go-kart that can reach speeds of more than 70 miles per hour, […]
Recent Comments